Fungal acne skincare routine—it’s something you may have heard of but aren’t exactly sure how to approach. Fungal acne, also known as pityrosporum folliculitis, is frequently misdiagnosed and confused with regular acne.
However, treating it requires a specific skincare routine designed to target the unique causes of fungal acne. In this guide, we will break down everything you need to know about fungal acne skincare routines, from understanding the condition to selecting the best, budget-friendly products for your skin.
Whether you’re dealing with the irritation of fungal acne or just want to prevent it, having a fungal acne skincare routine that is both effective and gentle is essential.
You don’t need to break the bank for quality products—let’s dive in and explore how you can tackle fungal acne without the guesswork!
Table of Contents
1. What is Fungal Acne?
Before diving into the fungal acne skincare routine, it’s crucial to understand what fungal acne is and how it differs from regular acne.
• Definition of Fungal Acne: Fungal acne is a skin condition caused by an overgrowth of the yeast Malassezia within the hair follicles, leading to breakouts that resemble traditional acne.
• How It Differs from Regular Acne: Although both fungal acne and regular acne cause pimples, fungal acne typically appears as uniform, small bumps, often on the forehead, chest, and back.
• Triggers: Fungal acne can be prompted by hot and humid conditions, excessive sweating, and the application of greasy or heavy skincare products.
• Why it’s tricky: Fungal acne may not respond well to traditional acne treatments like benzoyl peroxide or salicylic acid, which are meant for bacterial acne, not fungal infections. This is why it’s important to focus on treatments that target yeast overgrowth.
2. Identifying Fungal Acne: Common Signs & Symptoms
Fungal acne appears differently from regular acne, and identifying its symptoms is essential for effective treatment.
• Small, Uniform Bumps: Typically, the bumps are very uniform in size and form clusters, often appearing on the forehead, chest, back, or upper arms. These bumps are usually itchy.
• Itchy Sensation: Unlike regular acne, fungal acne may cause itching or discomfort. Itching refers as a key indicator pointing toward a fungal infection.
• Presence of Pimples on the Chest or Back: Fungal acne often affects areas other than the face, like the chest, neck, or back. If you notice similar bumps in these areas, it could be fungal acne.
• Inflammation: Sometimes, fungal acne can be inflamed and red. However, the inflammation tends to be less severe than with bacterial acne.
• Non-Inflammatory: Typically, there’s no whitehead or blackhead formation as seen in regular acne. Instead, you’ll see more flat or raised bumps that look similar to tiny pimples.
3. Treatment for Fungal Acne
When creating a fungal acne skincare routine, the key is targeting the yeast without irritating your skin.
Here are some effective treatments.
• Antifungal Creams or Shampoos: These are essential in fighting the yeast overgrowth. Products like ketoconazole or clotrimazole can be very effective when applied to the affected areas.
• Salicylic Acid: A mild exfoliator that can help remove dead skin cells, preventing clogged pores. However, be cautious not to overuse, as too much exfoliation can irritate the skin.
• Azelaic Acid: Known for its ability to reduce inflammation and fight acne, this ingredient can be especially effective for fungal acne, as it helps control both inflammation and yeast overgrowth.
• Topical Antibiotics: In some cases, your dermatologist may prescribe topical antibiotics to control inflammation or bacterial overgrowth in addition to fungal acne treatments.
• Oral Medication: In more severe cases, doctors may recommend antifungal oral medication like fluconazole to manage fungal acne when topical treatments aren’t enough.

4. How to Prevent Fungal Acne?
Prevention is always better than treatment. Here’s how to reduce the likelihood of fungal acne from occurring in the first place:
• Steer clear of overusing heavy skincare products: Thick and greasy formulations may worsen fungal acne. Opt for lighter, non-comedogenic options that don’t clog your pores.
• Stay Clean and Dry: Yeast thrives in warm, moist environments, so it’s important to keep your skin clean and dry, especially after workouts. A helpful tip is to shower promptly after exercising to help prevent sweat from accumulating on the skin.
• Use an Antifungal Cleanser: Incorporating a gentle antifungal cleanser into your routine can help prevent overgrowth. Products with ingredients like ketoconazole or zinc pyrithione are good options.
• Exfoliate Regularly: Exfoliating helps keep pores clean and free of dead skin, which reduces the risk of fungal growth. Choose an exfoliator with salicylic acid or gentle AHA formulas to slough off dead skin cells.
• Wear Breathable Fabrics: Especially for those who have fungal acne on the body, wearing fabrics that allow your skin to breathe—like cotton or moisture-wicking workout clothes—can help prevent flare-ups.
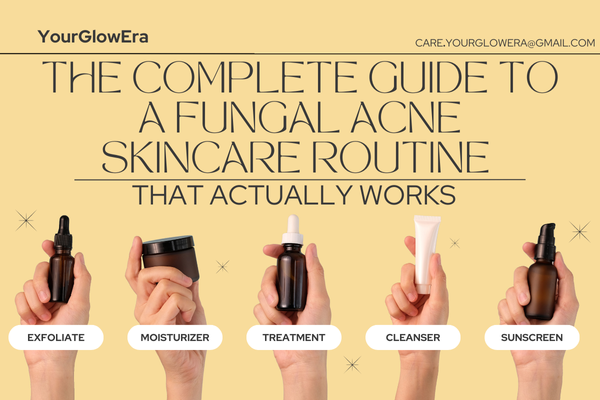
5. Fungal Acne Skincare Routine: Step-by-Step Process
Now that we know how to treat and prevent fungal acne, let’s put it all together into a simple, step-by-step skincare routine.
• Step 1: Cleanse
Begin with a mild, antifungal cleanser that effectively cleanses the skin without removing its natural oils. Opt for products with ketoconazole or zinc pyrithione to help kill the yeast responsible for fungal acne. It’s important to cleanse twice daily to keep your skin free of excess oil and dirt.
• Step 2: Exfoliate
Gently exfoliate with products containing salicylic acid to keep pores clear of dead skin and debris. This helps prevent fungal acne from forming in the first place by ensuring that your pores remain clean.
• Step 3: Apply Topical Treatment
If you have any fungal acne spots, apply antifungal creams or gels. Azelaic acid can also be used to treat areas with redness or inflammation, as it has both anti-inflammatory and antifungal properties.
• Step 4: Moisturize
Select a lightweight, oil-free moisturizer to maintain hydration while avoiding pore-clogging. Hydration is key, especially if you’re using drying treatments like salicylic acid or antifungal creams.
• Step 5: Sunscreen
Always finish with sunscreen. Exposure to the sun can worsen inflammation and irritation in fungal acne, so protect your skin with a lightweight, broad-spectrum SPF 30 or higher. Choose sunscreens marked as non-comedogenic to prevent pore blockage.
6. Choosing the Right Products for Your Fungal Acne Skincare Routine
Not all skincare products are made equal, especially when it comes to fungal acne. Here are some top recommendations:
• Cleansers: Look for those with antifungal properties, like Neutrogena’s anti-dandruff shampoo or Nizoral. These cleansers assist in removing the yeast responsible for fungal acne.
• Moisturizers: Stick to non-comedogenic, oil-free formulas like CeraVe or La Roche-Posay. These are gentle and hydrating, making them great for sensitive skin.
• Treatment Creams: Antifungal treatments like Lotrimin or Lamisil can be used for stubborn spots that aren’t responding to other treatments.
• Exfoliators: Products containing salicylic acid or gentle exfoliants like Paula’s Choice Skin Perfecting 2% BHA Liquid can help keep your pores clean without irritating your skin.
• Sunscreens: Opt for lightweight, oil-free sunscreens like EltaMD or Neutrogena Clear Face sunscreen to avoid clogging pores and to protect your skin from the harmful effects of UV rays.
7. Common Mistakes to Avoid in a Fungal Acne Skincare Routine
When managing fungal acne, it’s important to be aware of common mistakes that can hinder your progress.
Here are some common points to be aware of while dealing with fungal acne:
• Using Too Many Harsh Products: Excessive exfoliation or strong acne treatments can worsen fungal acne. It’s important to avoid products that may strip the skin of its natural oils, as this can cause more irritation.
• Skipping Antifungal Treatment: Don’t skip antifungal treatments—yeast is the root cause of fungal acne, and if you don’t address the fungal issue, it will continue to flare up.
• Overuse of Oil-Based Products: These can feed the yeast and make fungal acne worse. Stick to oil-free or water-based products.
• Not Using Sunscreen: Sun exposure can irritate fungal acne and make it worse. Sunscreen helps prevent additional inflammation and hyperpigmentation.
• Neglecting Body Acne: If you’re experiencing fungal acne on your body, be sure to treat those areas as well. This includes your chest, back, and even your arms.
8. How to Handle Fungal Acne Flare-Ups
Even with the best routine, flare-ups can still occur. Here’s how to handle them:
• Spot Treatment: Use antifungal ointments directly on affected areas to target the infection. Taking these precautions will help prevent the spread of the yeast and accelerate the healing of the spots.
• Hydration is Key: Make sure to keep your skin hydrated, especially if using drying products like antifungal treatments. Use an oil-free moisturizer to avoid clogging pores.
• Consult Your Dermatologist: If flare-ups are frequent or severe, it’s a good idea to consult with your dermatologist. They may recommend a stronger treatment regimen or oral antifungal medication.

9. Best Budget-Friendly Products for Fungal Acne
Taking care of fungal acne doesn’t have to be expensive. Here are some budget-friendly options that are effective and gentle on your skin:
• Nizoral Anti-Dandruff Shampoo: Works as both a body and facial cleanser. It contains ketoconazole, which is effective against fungal acne.
• CeraVe Hydrating Facial Cleanser: Affordable and gentle for everyday use. It provides hydration and does not remove moisture from the skin.
• Neutrogena Clear Face Sunscreen: Budget-friendly and non-comedogenic. This sunscreen is non-comedogenic and won’t clog pores or cause skin irritation.
• The Ordinary Azelaic Acid Suspension 10%: A budget-friendly and effective option for reducing inflammation and redness. This helps calm irritated skin while treating fungal acne.
10. Long-Term Management of Fungal Acne
Managing fungal acne isn’t just about treating flare-ups; it’s about long-term care. Here’s how to keep your skin healthy in the long run:
• Consistency is Key: Stick to your routine even when your skin improves. Consistency will prevent future breakouts and keep your skin clear.
• Monitor Your Skin’s Needs: Pay attention to what products work best for you, and don’t hesitate to adjust your routine if necessary.
• Continue Preventive Measures: Use antifungal cleansers and light, breathable fabrics regularly to keep fungal acne at bay.
Conclusion
In summary, a fungal acne skincare routine that actually works involves understanding your skin, using the right antifungal treatments, and selecting the right products.
By following a targeted fungal acne skincare routine that includes cleansing, exfoliating, moisturizing, and applying the right treatments, you can manage and prevent fungal acne effectively. Plus, you don’t have to spend a fortune—there are plenty of affordable options in your fungal acne skincare routine to achieve clear, healthy skin!
If you’re looking to build a skincare routine that specifically targets fungal acne, “How to Build a Fungal Acne Skincare Routine for Smooth and Clear Skin“ is the perfect guide for you. This detailed article will walk you through the essential steps you need to take to create an effective routine that works for your skin type and helps eliminate fungal acne.
The guide covers everything from choosing the right cleansers and treatments to understanding how to incorporate these products into your daily regimen.
With expert advice and product recommendations, you’ll have all the information you need to achieve smoother, clearer skin. Don’t miss out on these powerful tips – read the guide today and start building your fungal acne skincare routine!
Frequently Asked Questions
1. What is the root cause of fungal acne?
Fungal acne is caused by an overgrowth of the Malassezia yeast that naturally lives on the skin. This can be triggered by factors like oily skincare, sweating, and wearing tight clothing.
2. Why is my fungal infection not going?
If fungal acne isn’t improving, it may be due to incorrect treatment, inconsistent application, or ongoing exposure to triggers like sweat or oily skincare. Following a consistent fungal acne skincare routine and addressing these factors is key to seeing improvements.
3. Does glycolic acid help fungal acne?
Glycolic acid helps with exfoliation and cell turnover but does not have antifungal properties. While it can help with regular acne, it won’t target fungal acne directly. For effective fungal acne treatment, it’s important to follow a fungal acne skincare routine that includes antifungal ingredients.
4. Which serum is used to remove acne marks?
Serums containing ingredients like vitamin C, niacinamide, and retinoids are great for fading acne marks and improving skin texture, making them a valuable addition to your fungal acne skincare routine. These ingredients help promote skin healing while maintaining a clear complexion.
5. Is rose water good for fungal acne?
Rose water can soothe the skin, reduce redness, and help with hydration. It is generally safe for fungal acne, but it won’t directly treat the yeast overgrowth.
6. Does honey help fungal acne?
Honey has antibacterial and anti-inflammatory properties and can help soothe the skin. However, it is not antifungal and should not be relied on as the main treatment for fungal acne. For effective results, follow a proper fungal acne skincare routine with antifungal ingredients.
7. Which Moisturizer is best for fungal acne?
A lightweight, oil-free moisturizer such as CeraVe Daily Moisturizing Lotion or Neutrogena Hydro Boost is ideal for fungal acne-prone skin.
8. What is the difference between hormonal acne and fungal acne?
Hormonal acne is triggered by hormonal imbalances and usually appears as larger, cystic pimples. Fungal acne, on the other hand, consists of smaller, uniform bumps caused by yeast overgrowth.
9. What do dermatologists recommend for fungal acne?
Dermatologists typically recommend antifungal treatments like ketoconazole, miconazole, and selenium sulfide as part of a fungal acne skincare routine, along with gentle cleansers and oil-free moisturizers. These treatments help target yeast overgrowth, which is the primary cause of fungal acne.
10. Which hormone causes acne in females?
Androgens, male hormones found in both men and women, are known to increase sebum production, which can lead to clogged pores and acne, including fungal acne. Managing hormone levels and following a proper fungal acne skincare routine can help reduce the impact.
11. How long does it take to see results from a fungal acne skincare routine?
With consistent use of the right products, you may start to see improvement in 2-4 weeks. However, results vary depending on the severity of fungal acne and how strictly you follow your fungal acne skincare routine.
12. Should I see a dermatologist for fungal acne?
If over-the-counter treatments are not working, it’s a good idea to consult a dermatologist. They can prescribe stronger antifungal treatments and guide you on how to adjust your fungal acne skincare routine for the best results.
13. Can fungal acne affect areas other than the face?
Yes, fungal acne skincare routine is essential as fungal acne can appear on other parts of the body, such as the back, chest, shoulders, and arms. It thrives in warm, sweaty environments, so areas that are often covered or sweat-prone are common spots for fungal acne. A proper routine can help prevent and treat it effectively.







Leave a reply